Will it create health problems decades from now?
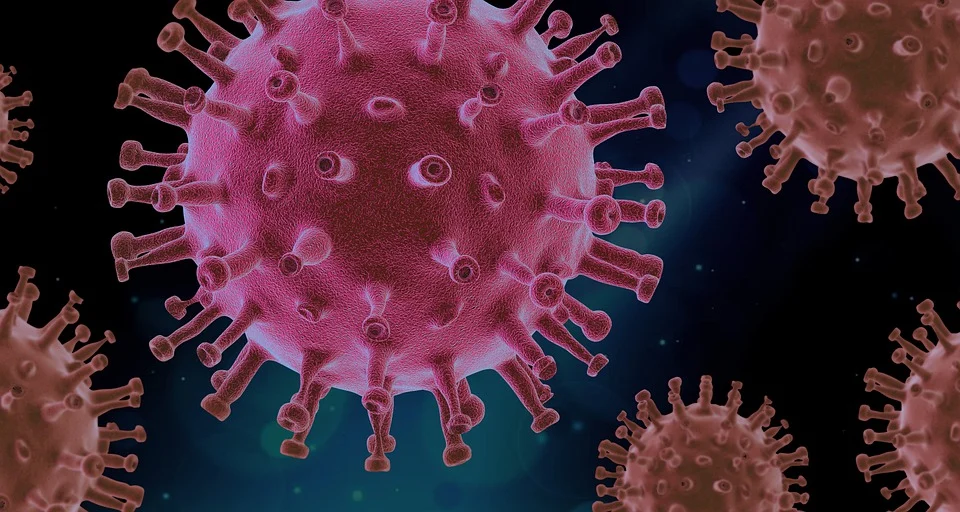
In the early days of 2020, the ailment was labeled “pneumonia of unknown source,” but it has proven to be considerably more bizarre.
We now know, two years into the epidemic, that COVID-19 may cause a baffling mix of symptoms, ranging from heart inflammation to brain fog to loss of smell or taste. Some people’s toes become red, while some individuals acquire diabetes.
SARS-CoV-2 also affects several organs and may result in long-term respiratory issues, tiredness, or chronic renal damage.
Time and study have shown that the virus has a proclivity for wreaking havoc on the human body under the correct circumstances.
So, what does this indicate for the long-term health of millions of infected individuals – months, years, or even decades down the road?
Matthew Miller, an associate professor at McMaster University’s Immunology Research Centre in Hamilton added there are certain ‘known’ unknowns, such as what the rate and duration of long COVID will be for various people, and there are the ‘unknown’ unknowns, such as what may happen in 30 or 50 years.
Diabetes-Related Infections and Neurological Problems
The capacity of SARS-CoV-2 to spread throughout the body is partly due to spike proteins on its surface, which attach to ACE2 — a protein found on the surface of numerous kinds of human cells — like a key into a lock.
That implies the virus has the potential to travel far beyond the respiratory system, producing inflammation everywhere it goes.
When it comes to extended COVID, the therapeutic strategy is always changing.
It has been shown that this virus, even in the acute stage, has an impact on the brain and our central organs like the heart and pancreas, and areas where other viral infections have caused longer-term inflammatory changes that have led to chronic disease, as stated by Dr. Cory Neudorf, co-lead of the public health, health systems, and social policy impacts pillar for CoVaRR-Net, a team of Canadian researchers who banded together during the pandemic.
He added he wouldn’t be shocked if we see more chronic disorders as a result of COVID in the next years.
That implies the virus has the potential to travel far beyond the respiratory system, producing inflammation everywhere it goes.
In addition to the immediate effects of a SARS-CoV-2 infection, which may send some patients to the hospital, the virus can occasionally cause long-term respiratory issues, exhaustion, or chronic kidney damage.
Two infections have been associated with the development of diabetes in children.
According to a January research from the Centers for Disease Control and Prevention, adolescents under the age of 18 were more likely to be diagnosed with diabetes a month or more after infection than young people who did not have COVID-19 — and when compared to respiratory illnesses before to the pandemic.
These results are consistent with prior studies suggesting a connection between SARS-CoV-2 infection and diabetes in adults, as written by the article.
Other studies have connected even modest COVID-19 infections to long-term neurological problems.
One recent U.S. research, which has not yet been peer-reviewed, included autopsy data from nine patients as well as an investigation of the effects on lab mice infected with SARS-CoV-2 on purpose.
As Alberta faces the 5th wave of COVID-19, hospitals are seeing an influx of youngsters.
Scientists discovered that the very mild, acute course of SARS-CoV-2 in this mouse model induces substantial neuro-inflammation, as stated by lead researcher Michelle Monje, a neurology professor at Stanford University in California, in an interview with CBC News.
The research thinks that this is what causes the “brain fog” reported by some individuals after an episode of COVID-19, which is similar to what some people feel after chemotherapy treatment.
Persistent Symptoms Might Be ‘Debilitating’
The sensation of post-infection brain fog, coupled with other lasting consequences, is referred to as protracted COVID – a well-documented but yet poorly understood phenomenon.
As co-lead investigator for the Canadian COVID-19 Prospective Cohort Study, Dr. Angela Cheung, a senior scientist-clinician at the University Health Network in Toronto, has spent most of the pandemic dealing with long COVID patients.
She described patients’ symptoms as “all over the place,” ranging from acute tiredness to heart palpitations to sleep disturbance.
Miller, the McMaster researcher, is especially worried about long-term health effects that appear immediately after infection and seem to last for extended periods of time, “or potentially even for life.”
Conclusion
Let us not play Russian roulette with Omicron by accepting it as unavoidable.
Nonetheless, considering all of the unknowns surrounding this coronavirus and how little time has elapsed since it started spreading among humans, Miller believes huge uncertainties remain about how infections may impact individuals in the future.
Miller noted:
“An infection compounded on top of that genetic predisposition might be enough to tip the scale, so that person experiences a disease that they might not have experienced otherwise.”












Leave a Reply